The low FODMAP diet in practice

The following case study is based on a generic patient using epidemiological data and the following references and any similarity to individual cases is purely coincidental.
Mrs Smith is 46 and in 1997 had an episode of traveller’s diarrhoea whilst on holiday; she was referred by her GP to the gastroenterologist for investigation in 1998 after presenting with weight loss, diarrhoea and abdominal pain. Her tissue transglutaminase (IgA tTG) coeliac screen was negative and small bowel biopsy was normal whilst consuming at least 6 weeks of a gluten containing diet, she had no bowel infection or parasitic infestation. Her inflammatory markers and faecal calprotectin test (showing bowel inflammation), which were tested more recently, were normal. Her colonoscopy, SeHCAT test, faecal elastase and lactose breath test were also normal. She has no history of eczema, asthma or atopy and had no previous abdominal surgery.
She was discharged to primary care after extensive work up with a diagnosis of IBS-D and prescribed Loperamide Hydrochloride and Mebeverine Hydrochloride for symptomatic control, she used these occasionally. She is a frequent user of primary care services and found the process of reaching a diagnosis caused anxiety at the time and was both frustrating and unhelpful for her.
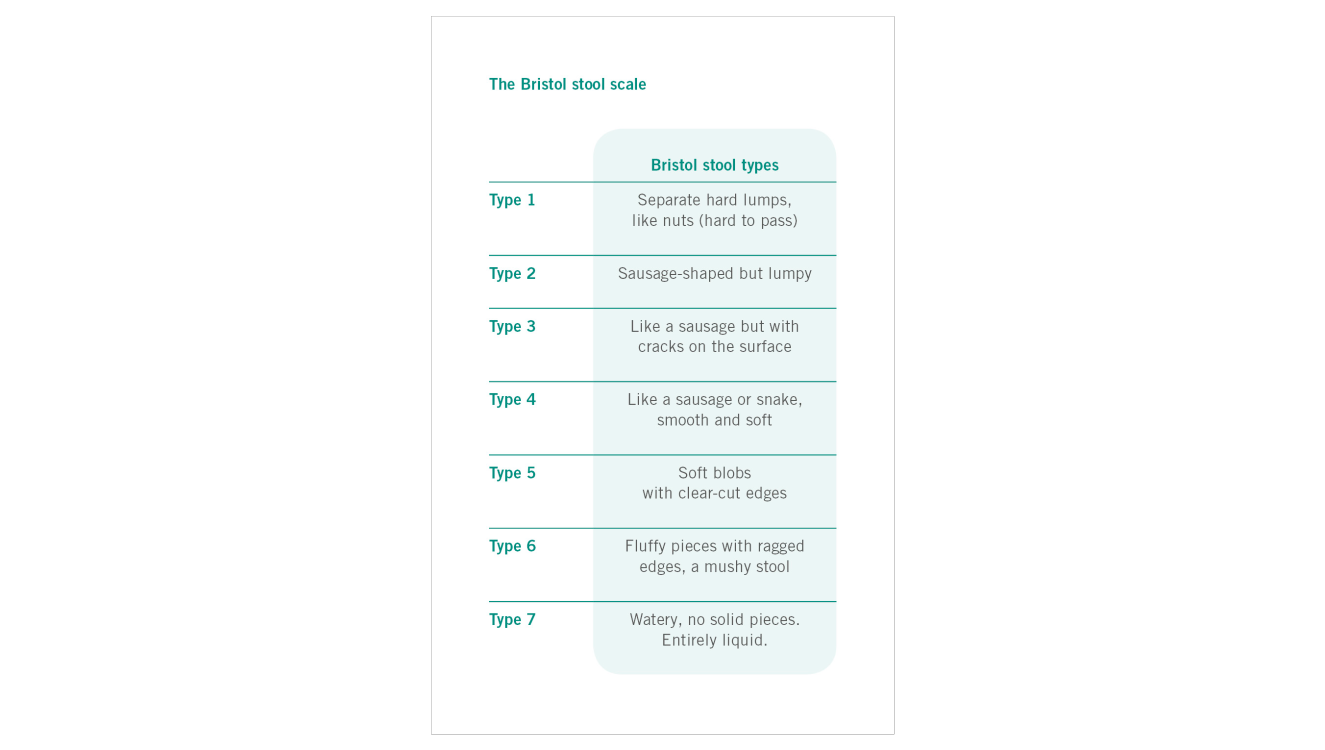
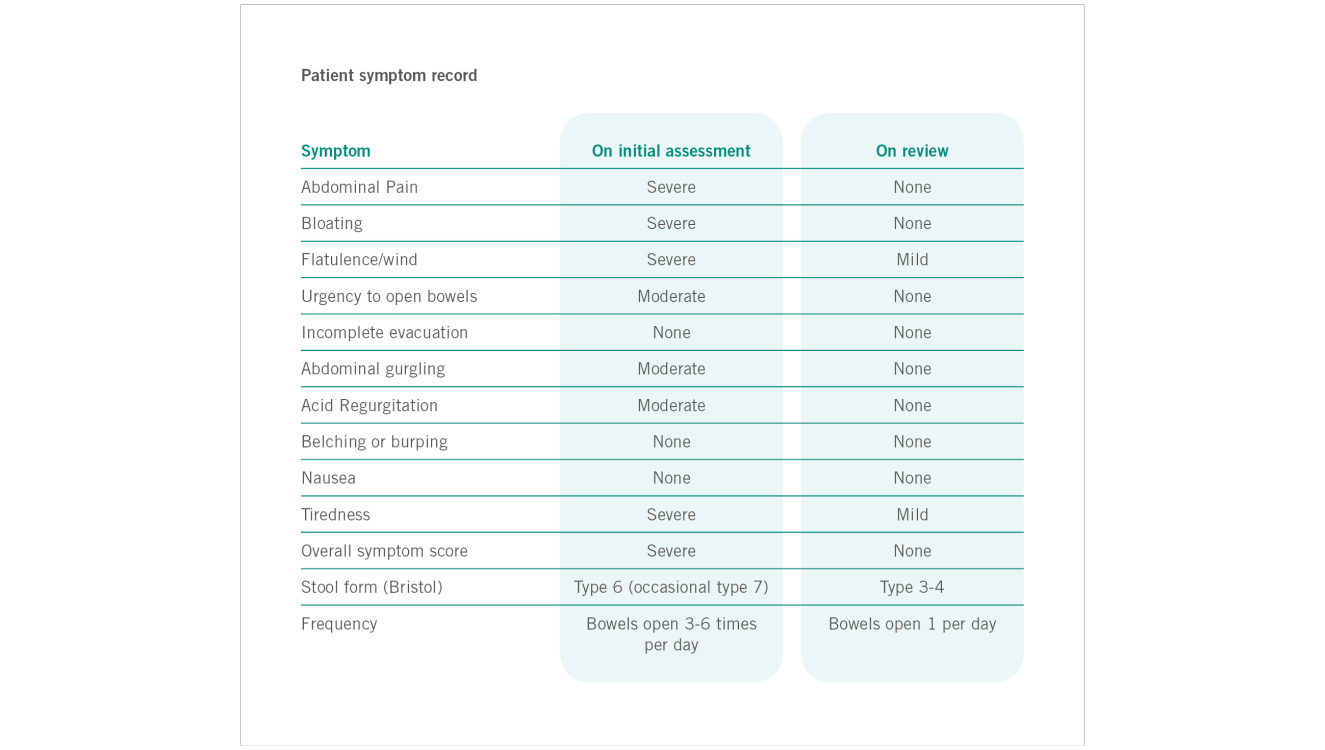
On her last visit to her GP she informed her that she had tried the Low FODMAP diet after researching it on the internet and whilst she felt her symptoms had improved to a small degree, the information she downloaded on the diet was often inconsistent and confusing. She therefore requested a referral to a FODMAP trained dietitian to try the diet in a more systematic manner. On initial assessment Mrs Smith was given an explanation of IBS-D as a functional gut disorder and the role of gastroenterology and the Rome III criteria in the positive diagnosis of IBS and asked if she was happy to discuss her symptoms. Her symptoms were assessed using a symptom assessment tool based on the gastrointestinal symptom rating scale (GSRS, Svedlund et al., 1988), the Bristol stool chart and a global symptom question (see symptom chart) her current medical, family and social history were queried; weight, weight history, diet and any foods avoided were also queried and discussed. She was prescribed 2 months exclusion of high FODMAP foods except lactose, which was not problematic.
She was discharged to primary care after extensive work up with a diagnosis of IBS-D and prescribed Loperamide Hydrochloride and Mebeverine Hydrochloride for symptomatic control, she used these occasionally. She is a frequent user of primary care services and found the process of reaching a diagnosis caused anxiety at the time and was both frustrating and unhelpful for her.
On her last visit to her GP she informed her that she had tried the Low FODMAP diet after researching it on the internet and whilst she felt her symptoms had improved to a small degree, the information she downloaded on the diet was often inconsistent and confusing. She therefore requested a referral to a FODMAP trained dietitian to try the diet in a more systematic manner. On initial assessment Mrs Smith was given an explanation of IBS-D as a functional gut disorder and the role of gastroenterology and the Rome III criteria in the positive diagnosis of IBS and asked if she was happy to discuss her symptoms. Her symptoms were assessed using a symptom assessment tool based on the gastrointestinal symptom rating scale (GSRS, Svedlund et al., 1988), the Bristol stool chart and a global symptom question (see symptom chart) her current medical, family and social history were queried; weight, weight history, diet and any foods avoided were also queried and discussed. She was prescribed 2 months exclusion of high FODMAP foods except lactose, which was not problematic.
On review she reported it took approximately six weeks for her symptoms to improve significantly and she was following the diet well. Initially she was reluctant to go ahead with re-introduction as she had satisfactory symptom relief, but decided to when it was explained that it might not be all FODMAP containing foods that would result in symptoms and having more variety would be helpful to manage her diet. After the re-introduction process she found fructans and fructose problematic and was excluding these foods from her diet, but her diet was otherwise varied and nutritionally balanced and she was ultimately discharged from care.
Author
JULIE THOMPSON
is a HCPC Clinical Lead Dietitian working in the NHS and private practice. She has an interest in gastroenterology and has experience in treatment of food intolerances and dietary treatment of conditions such as irritable bowel syndrome (IBS), Crohn’s disease, colitis and coeliac disease. She is an executive on the board of The IBS Network, the UK charity for people with IBS and has experience in treatment of irritable bowel syndrome with diet, including being trained to use The Low FODMAP dietary approach to reduce functional bowel symptoms. She has written for the Guardian, Sainsbury’s Magazine, Network Health Dietitians Magazine and GUT Reaction.
is a HCPC Clinical Lead Dietitian working in the NHS and private practice. She has an interest in gastroenterology and has experience in treatment of food intolerances and dietary treatment of conditions such as irritable bowel syndrome (IBS), Crohn’s disease, colitis and coeliac disease. She is an executive on the board of The IBS Network, the UK charity for people with IBS and has experience in treatment of irritable bowel syndrome with diet, including being trained to use The Low FODMAP dietary approach to reduce functional bowel symptoms. She has written for the Guardian, Sainsbury’s Magazine, Network Health Dietitians Magazine and GUT Reaction.
References
- Canavan C., West J., Card T. (2014) The Epidemiology of Irritable Bowel Syndrome. Clinical Epidemiology 2014;6:71–80
- Staudacher H. M., Whelan K., Irving P. M., Lomer M. C. E. (2011) Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. Journal of Human Nutrition & Dietetics
- Mackenzie et al. (2012) British Dietetic Association evidence-based guidelines for dietary treatment of Irritable Bowel syndrome in Adults. Journal of Human Nutrition & Dietetics
- Svedlund J., Sjodin I., Dotevall G. (1988) GSRS – a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig Dis Sci. 1988;33:129–134
www.drschaer-institute.com
