The Global Phenomenon of Self-Reported Wheat Sensitivity
Imran Aziz. Editorial. American Journal of Gastroenterology 2018.
There is recognition that the prevalence of coeliac disease, the most commonly recognised gluten-related disorder, is higher than previously thought and is potentially rising. The change in prevalence may be due to increasing immunogenicity of gluten but also through improved diagnosis and a shift in understanding of coeliac disease. In the last ten years, the availability of gluten-free foods and awareness of gluten-related disorders has changed dramatically. Public demand and adoption of a gluten-free diet (GFD) as a lifestyle option have been the main drivers of this. However, the scientific community had remained largely sceptical regarding the uptake of a GFD until the publication of a key paper demonstrating that gluten-based products induced symptoms in the absence of coeliac disease, resulting in a change in mindset. Yet, controversy remains as to which component of wheat causes symptoms. Given the absence of biomarkers and the problematic nature of undertaking double-blind, placebo-controlled challenges in clinical practice, this condition is increasingly being referred to as ‘self-reported wheat sensitivity’ (SRWS) and in those where coeliac disease has been excluded ‘self-reported non-coeliac wheat sensitivity’ (SR-NCWS).
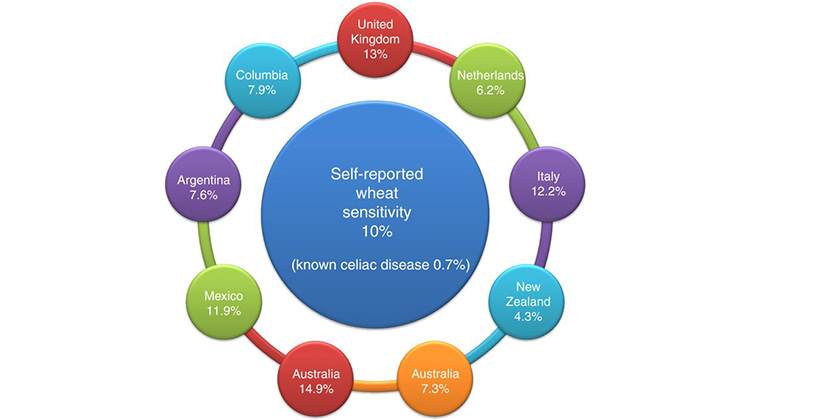
The pooling of results from a number of observational studies from different countries, looking at SRWS, demonstrate an average prevalence of 10% (range 4.3-14.9%). The clinical phenotype is typically young to middle-aged women who attribute their intestinal or extra intestinal symptoms to the ingestion of wheat. Intestinal and extra intestinal symptoms are both reported with many fulfilling the criteria for IBS.
A novel observation from a newly-published study found a strong association between SRWS and symptom-based Rome III functional dyspepsia, with 31.3% of subjects with SRWS fulfilling the criteria for functional dyspepsia compared to 13.6% in those without SRWS. Based on previous research the authors speculated that wheat may be the environmental allergen implicated in functional dyspepsia which affects approximately 10% of the population and of which postprandial distress syndrome represents the majority. This is acknowledged as an association not a causation and further research is required. An alternative view could be that the high-residue content of a wheat-based diet exacerbates symptoms in patients with postprandial distress syndrome, which is characterised by early satiety and fullness. There are also questions as to whether a wheat-based immune reaction drives inflammatory bowel disease (IBD), or more plausibly, that IBD is symptomatic to the high-residue content and fermentation properties of wheat, as SR-NCWS is common in those with severe or structuring IBD. In IBS, where upto 25% of patients have SR-NCWS, the direction of causality is not necessarily straightforward. In most, it appears that a wheat-based diet provokes the underlying dysfunctional gut-brain axis of IBS through the fermentation of fructans. However, in a subset symptoms may be the result of gluten as demonstrated by intestinal cell damage, altered barrier function, elevated gliadin antibodies, increased systemic immune activation, which reverses on a GFD and provides symptom improvement.
From a clinician perspective, it is important to initially exclude CD and thus diagnose SR-NCWS. In those already on a GFD, a negative HLA-DQ2/8 excludes CD, which is the case in approximately 50%. If the patient is HLA-DQ2/8 positive, then a discussion regarding a gluten challenge prior to proceeding to serological tests and duodenal biopsies should be covered. Recent research suggests that the HLA-DQ- gluten tetramer blood test, which accurately identifies patients with or without CD even in the absence of gluten consumption, may be the best approach in this situation although further validation studies are required. It is also currently unclear as to how best to manage these
Link to full study: https://doi.org/10.1038/s41395-018-0103-y
The pooling of results from a number of observational studies from different countries, looking at SRWS, demonstrate an average prevalence of 10% (range 4.3-14.9%). The clinical phenotype is typically young to middle-aged women who attribute their intestinal or extra intestinal symptoms to the ingestion of wheat. Intestinal and extra intestinal symptoms are both reported with many fulfilling the criteria for IBS.
A novel observation from a newly-published study found a strong association between SRWS and symptom-based Rome III functional dyspepsia, with 31.3% of subjects with SRWS fulfilling the criteria for functional dyspepsia compared to 13.6% in those without SRWS. Based on previous research the authors speculated that wheat may be the environmental allergen implicated in functional dyspepsia which affects approximately 10% of the population and of which postprandial distress syndrome represents the majority. This is acknowledged as an association not a causation and further research is required. An alternative view could be that the high-residue content of a wheat-based diet exacerbates symptoms in patients with postprandial distress syndrome, which is characterised by early satiety and fullness. There are also questions as to whether a wheat-based immune reaction drives inflammatory bowel disease (IBD), or more plausibly, that IBD is symptomatic to the high-residue content and fermentation properties of wheat, as SR-NCWS is common in those with severe or structuring IBD. In IBS, where upto 25% of patients have SR-NCWS, the direction of causality is not necessarily straightforward. In most, it appears that a wheat-based diet provokes the underlying dysfunctional gut-brain axis of IBS through the fermentation of fructans. However, in a subset symptoms may be the result of gluten as demonstrated by intestinal cell damage, altered barrier function, elevated gliadin antibodies, increased systemic immune activation, which reverses on a GFD and provides symptom improvement.
From a clinician perspective, it is important to initially exclude CD and thus diagnose SR-NCWS. In those already on a GFD, a negative HLA-DQ2/8 excludes CD, which is the case in approximately 50%. If the patient is HLA-DQ2/8 positive, then a discussion regarding a gluten challenge prior to proceeding to serological tests and duodenal biopsies should be covered. Recent research suggests that the HLA-DQ- gluten tetramer blood test, which accurately identifies patients with or without CD even in the absence of gluten consumption, may be the best approach in this situation although further validation studies are required. It is also currently unclear as to how best to manage these
Link to full study: https://doi.org/10.1038/s41395-018-0103-y
www.drschaer-institute.com
