The influence of the microbiome on gluten-related diseases

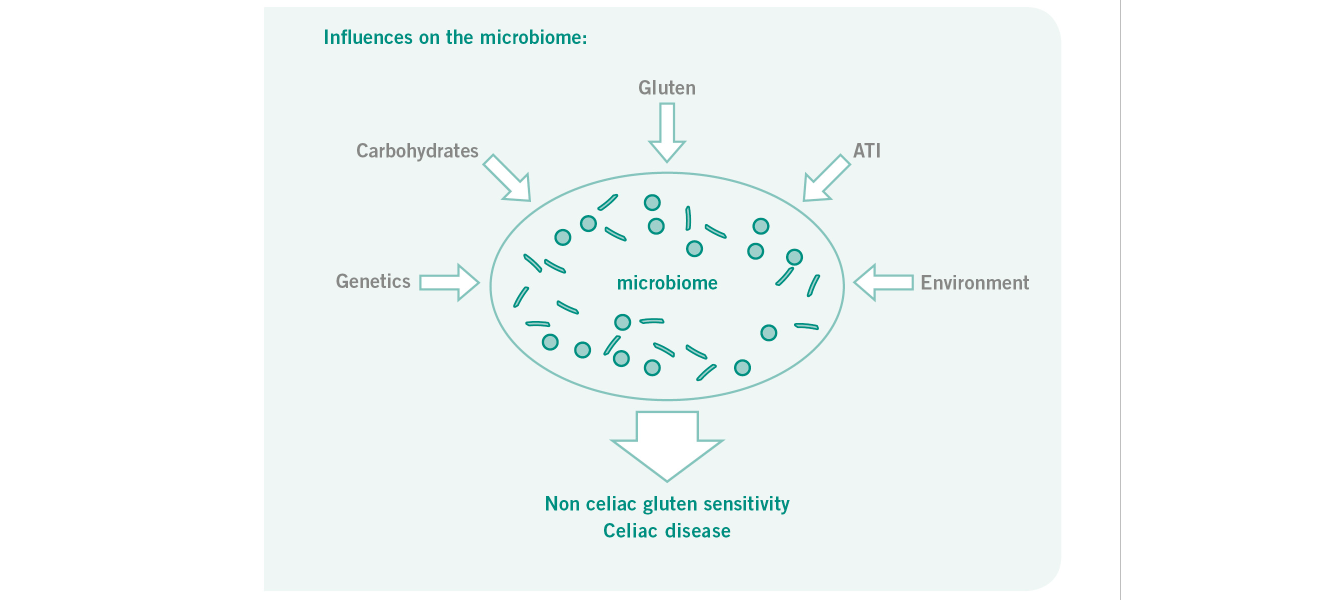
The increasing prevalence of food intolerances, especially in relation to certain carbohydrates, represents a global health problem. [1] Moreover, intolerance of gluten and gluten-bound substances, e.g. amylase-trypsin inhibitor (ATI) is blamed [2] for intestinal (e.g. meteorism, pain, constipation, diarrhea) and extra intestinal symptoms (e.g. fatigue, headaches, joint pain, skin irritation) in affected patients. [3] The pathogenesis of food intolerances is blamed on factors such as changes in the composition of the intestinal flora and its influence on mucous membrane immune tolerance. [4]
The intestinal barrier is important to maintain homoeostasis in the intestine. If intestinal imbalance occurs, the intestinal barrier can be attacked and become permeable as part of leaky gut syndrome. It has been proven that there is an association between leaky gut syndrome and the development of gastrointestinal disease and possibly food intolerances. [5]
The microbiome of the human digestive tract therefore also appears to play an important role in influencing wheat/gluten-associated disease. [4]
It is common knowledge that the intestinal microflora is dependent on many factors. The microbial composition in the small intestine is primarily determined by the competition between micro-organisms and the host to ensure rapid absorption and utilization of carbohydrates. The micro-organisms in the colon, on the other hand, are affected by both the complex utilization of carbohydrates and competition among themselves. [6]
Nutrition plays an important role in this case. Mouse studies have already demonstrated that diet can rapidly alter the intestinal microbial composition. [7]
Numerous publications demonstrate the presence of streptococcus sp., E.coli, clostridium sp., GC-rich organisms, bacteroides uniformis, blautia glucerasea and bifidobacteria in the small and large intestine, which prefer different substrates. [8] It is interesting in this context that B. uniformis primarily utilises inulin, whereas other species primarily metabolise fructo-oligosaccharides or monosaccharides. [9] An indication of the importance of microbial composition in celiac disease is provided by the fact that there is a different bacterial population in these patients compared to non celiac individuals. A significantly higher proportion of bifidobacterium bifidum and increased numbers of lactobacillus sp. were found in celiac patients, but their diversity decreased significantly after maintaining a gluten-free diet. [10] Furthermore, it was demonstrated in-vitro that certain bifidobacterium strains reduced the inflammatory immune response triggered by gliadin peptides, thus exerting a protective effect. [11,12]
In 2013, Wacklin et al. reported a possible link between the manifestation of celiac disease in the form of gastrointestinal or extraintestinal symptoms and the microbiome. [13]
In another study, the duodenal microbiome of celiac disease patients with persistent symptoms despite long-term GFD and normalized small-intestinal mucosa was studied in comparison with celiac disease patients without symptoms. It was determined that there were differences in bacterial colonization of the small intestine between patients without symptoms and patients with persistent symptoms. They had a significantly increased amount of proteobacteria, whereas the number of bacteroidetes and firmicutes was reduced. Overall, the celiac disease patients with persistent symptoms exhibited reduced microbial diversity. In some subgroups of celiac disease there is thus evidence of a dysbiosis as a possible cause of recurrent symptoms, in which case new treatment approaches, e.g. in the form of pro- or prebiotics, would be possible. [14]
In addition, Smecuol et al. have already investigated the effect of the probiotic bifidobacterium infantis Natren Life Start Strain Super Strain on the clinical progress of untreated celiac patients. Of the 22 patients, 12 were given 2 B. infantes capsules and 10 were given 2 placebo capsules with meals. While taking the probiotic had no effect on intestinal permeability, symptoms of dyspepsia, constipation and gastro-esophageal reflux improved significantly in the B. infantis group. There was also a significant increase in MIP-1ß (macrophage inflammatory protein-1ß) in the probiotics group. Although this study indicates a possible mitigating effect of probiotics on some celiac disease symptoms, it requires confirmation by further studies. [15]
A recent study by Olivares et al. in patients with a high genetic risk of celiac disease revealed an altered microbial composition even in infancy and early childhood, which is an indication that the change in the microbiome might take place at a very early stage. Compared to infants without increased celiac risk, those individuals who were positive HLA-DQ2 carriers had a significantly higher number of firmicutes and proteobacteria, and a smaller number of actinobacteria. The number of bifidobacteria species was also reduced. A genetic predisposition in the form of HLADQ2 thus appears to have an impact on the microbiome and could as such also contribute to the pathogenesis. This finding could be useful in determining the risk of celiac disease. [16]
Generally, this data indicates that a link exists between the pathogenesis and the symptoms of gluten-related diseases and the human microbiome. However, the extent to which certain bacterial species are involved in the pathogenesis of celiac disease or NCGS, and the extent to which damaged mucosa provide preferential living conditions for these bacterial species, is still unclear and requires further investigation. The initial data from Biesiekierski et al. (2013) allows us to speculate that fermentable carbohydrates are also the cause or at least an influencing factors in patients with NCGS. We therefore consider determination of the microbial colonisation of very interesting for the detection of any differences between these patients and healthy controls.
In the context of a controlled prospective study, we are therefore examining changes in intestinal microflora in patients with documented NCGS with a mixed diet, gluten-free diet and low-FODMAP diet to determine the influence of carbohydrate chains on bacterial growth and differentiation thereof. The comparison with a healthy control group and a control population with proven celiac disease is used for better differentiation between the bacterial strains that are responsible for the pathogenesis of NCGS.
The detection of a specific flora composition in patients with NCGS could represent an innovative approach for targeted probiotic treatment with few side effects.
The microbiome of the human digestive tract therefore also appears to play an important role in influencing wheat/gluten-associated disease. [4]
It is common knowledge that the intestinal microflora is dependent on many factors. The microbial composition in the small intestine is primarily determined by the competition between micro-organisms and the host to ensure rapid absorption and utilization of carbohydrates. The micro-organisms in the colon, on the other hand, are affected by both the complex utilization of carbohydrates and competition among themselves. [6]
Nutrition plays an important role in this case. Mouse studies have already demonstrated that diet can rapidly alter the intestinal microbial composition. [7]
Numerous publications demonstrate the presence of streptococcus sp., E.coli, clostridium sp., GC-rich organisms, bacteroides uniformis, blautia glucerasea and bifidobacteria in the small and large intestine, which prefer different substrates. [8] It is interesting in this context that B. uniformis primarily utilises inulin, whereas other species primarily metabolise fructo-oligosaccharides or monosaccharides. [9] An indication of the importance of microbial composition in celiac disease is provided by the fact that there is a different bacterial population in these patients compared to non celiac individuals. A significantly higher proportion of bifidobacterium bifidum and increased numbers of lactobacillus sp. were found in celiac patients, but their diversity decreased significantly after maintaining a gluten-free diet. [10] Furthermore, it was demonstrated in-vitro that certain bifidobacterium strains reduced the inflammatory immune response triggered by gliadin peptides, thus exerting a protective effect. [11,12]
In 2013, Wacklin et al. reported a possible link between the manifestation of celiac disease in the form of gastrointestinal or extraintestinal symptoms and the microbiome. [13]
In another study, the duodenal microbiome of celiac disease patients with persistent symptoms despite long-term GFD and normalized small-intestinal mucosa was studied in comparison with celiac disease patients without symptoms. It was determined that there were differences in bacterial colonization of the small intestine between patients without symptoms and patients with persistent symptoms. They had a significantly increased amount of proteobacteria, whereas the number of bacteroidetes and firmicutes was reduced. Overall, the celiac disease patients with persistent symptoms exhibited reduced microbial diversity. In some subgroups of celiac disease there is thus evidence of a dysbiosis as a possible cause of recurrent symptoms, in which case new treatment approaches, e.g. in the form of pro- or prebiotics, would be possible. [14]
In addition, Smecuol et al. have already investigated the effect of the probiotic bifidobacterium infantis Natren Life Start Strain Super Strain on the clinical progress of untreated celiac patients. Of the 22 patients, 12 were given 2 B. infantes capsules and 10 were given 2 placebo capsules with meals. While taking the probiotic had no effect on intestinal permeability, symptoms of dyspepsia, constipation and gastro-esophageal reflux improved significantly in the B. infantis group. There was also a significant increase in MIP-1ß (macrophage inflammatory protein-1ß) in the probiotics group. Although this study indicates a possible mitigating effect of probiotics on some celiac disease symptoms, it requires confirmation by further studies. [15]
A recent study by Olivares et al. in patients with a high genetic risk of celiac disease revealed an altered microbial composition even in infancy and early childhood, which is an indication that the change in the microbiome might take place at a very early stage. Compared to infants without increased celiac risk, those individuals who were positive HLA-DQ2 carriers had a significantly higher number of firmicutes and proteobacteria, and a smaller number of actinobacteria. The number of bifidobacteria species was also reduced. A genetic predisposition in the form of HLADQ2 thus appears to have an impact on the microbiome and could as such also contribute to the pathogenesis. This finding could be useful in determining the risk of celiac disease. [16]
Generally, this data indicates that a link exists between the pathogenesis and the symptoms of gluten-related diseases and the human microbiome. However, the extent to which certain bacterial species are involved in the pathogenesis of celiac disease or NCGS, and the extent to which damaged mucosa provide preferential living conditions for these bacterial species, is still unclear and requires further investigation. The initial data from Biesiekierski et al. (2013) allows us to speculate that fermentable carbohydrates are also the cause or at least an influencing factors in patients with NCGS. We therefore consider determination of the microbial colonisation of very interesting for the detection of any differences between these patients and healthy controls.
In the context of a controlled prospective study, we are therefore examining changes in intestinal microflora in patients with documented NCGS with a mixed diet, gluten-free diet and low-FODMAP diet to determine the influence of carbohydrate chains on bacterial growth and differentiation thereof. The comparison with a healthy control group and a control population with proven celiac disease is used for better differentiation between the bacterial strains that are responsible for the pathogenesis of NCGS.
The detection of a specific flora composition in patients with NCGS could represent an innovative approach for targeted probiotic treatment with few side effects.
Authors
PROF. DR. MED. YURDAGÜL ZOPF
Medical Clinic 1, University of Erlangen, Germany
PRIV. DOZ. DR. RER. NAT. WALBURGA DIETERICH
Scientific employee Medical Clinic 1 University Erlangen, Germany
Medical Clinic 1, University of Erlangen, Germany
PRIV. DOZ. DR. RER. NAT. WALBURGA DIETERICH
Scientific employee Medical Clinic 1 University Erlangen, Germany
References
- Zopf Y. et al., The differential diagnosis of food intolerance. Dtsch Arztebl Int. 2009 May;106(21):359-69;
- Junker Y. et al., Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J Exp Med. 2012 Dec 17;209(13):2395-408.
- Volta U. et al., Non-celiac gluten sensitivity: questions still to be answered despite increasing awareness. Cell Mol Immunol. 2013 Sep;10(5):38392.
- Galipeau HJ, Verdu EF. Gut microbes and adverse food reactions: Focus on gluten related disorders. Gut Microbes. 2014;5(5):594-605.
- Barbara G. et al., Mucosal permeability and immune activation as potential therapeutic targets of probiotics in irritable bowel syndrome. J Clin Gastroenterol. 2012 Oct;46 Suppl:S52-5.
- Zoetendal, E.G. and W.M. de Vos, Effect of diet on the intestinal microbiota and its activity. Curr Opin Gastroenterol, 2014.
- Ooi, J.H., et al., Dominant effects of the diet on the microbiome and the local and systemic immune response in mice. PLoS One, 2014. 9(1): p. e86366.
- Zoetendal, E.G., et al., The human small intestinal microbiota is driven by rapid uptake and conversion of simple carbohydrates. ISME J, 2012. 6(7): p. 1415-26.
- Tannock, G.W., et al., RNA-stable isotope probing (RNA-SIP) shows carbon utilization from inulin by specific bacterial populations in the large bowel of rats. Appl Environ Microbiol, 2014.
- Nistal, E., et al., Differences in faecal bacteria populations and faecal bacteria metabolism in healthy adults and celiac disease patients. Biochimie, 2012. 94(8): p. 1724-9.
- Medina, M., et al., Bifidobacterium strains suppress in vitro the pro-inflammatory milieu triggered by the large intestinal microbiota of coeliac patients. J Inflamm (Lond), 2008. 5: p. 19.
- Laparra, J.M. and Y. Sanz, Bifidobacteria inhibit the inflammatory response induced by gliadins in intestinal epithelial cells via modifications of toxic peptide generation during digestion. J Cell Biochem, 2010. 109(4): p. 801-7.
- Wacklin, P., et al., The duodenal microbiota composition of adult celiac disease patients is associated with the clinical manifestation of the disease. Inflamm Bowel Dis, 2013. 19(5): p. 934-41.
- Wacklin, P., et al., Altered duodenal microbiota composition in celiac disease patients suffering from persistent symptoms on a long-term gluten-free diet. Am J Gastroenterol, 2014. 109(12): p. 1933-41.
- Smecuol E, H.H., Sugai E, Corso L, Cherñavsky AC, Bellavite FP, González A, Vodánovich F, Moreno ML, Vázquez H, Lozano G, Niveloni S, Mazure R, Meddings J, Mauriño E, Bai JC., Exploratory, randomized, double-blind, placebo-controlled study on the effects of Bifidobacterium infantis natren life start strain super strain in active celiac disease. J Clin Gastroenterol, 2013. 47: p. 139147.
- Olivares, M., et al., The HLA-DQ2 genotype selects for early intestinal microbiota composition in infants at high risk of developing coeliac disease. Gut, 2015. 64(3): p. 406-17.
www.drschaer-institute.com
